Leveraging Advanced Optometry Technology in Gosford
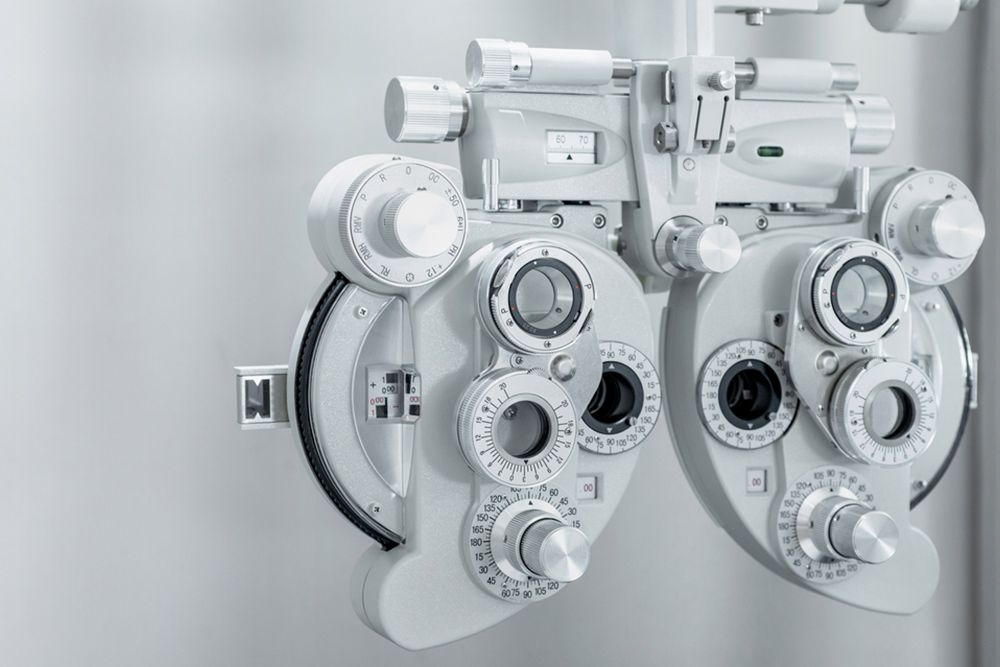
Modern Diagnostic & Treatment Technology
At Central Coast Eyecare in Gosford, we provide comprehensive eye care services using advanced optometry technology. We ensure our equipment is meticulously well-maintained and we put your comfort and health first when you visit us for an appointment.
Our OCULUS Dry Eye Suite allows us to diagnose and treat inflamed and irritable eyes by conducting a detailed analysis of tear film quality, meibomian gland function and corneal health. With precise tear film evaluation and corneal staining techniques, we can identify the root causes of dry eye conditions accurately.
Examples of other technologies we use include Optical Coherence Tomography (OCT) scanners for early disease detection, corneal topography assessors and automated perimetry technology. The equipment we use is designed to provide the best possible data regarding your vision and eye comfort, allowing us to personalise the optimal treatment plan.
If you have any questions about our technology, or you’d like to book a consultation contact our stores located in
Gosford,
Erina and
Killarney Vale.
Examples of Our Technology
The technology available at each of our offices includes the following:
OCULUS Dry Eye Suite:
This technology encompasses cutting-edge diagnostic tools for in-depth analysis of tear film, corneal health and meibomian glands. It enables precise evaluation of tear quality, quantity and stability, essential for identifying dry eye causes. Corneal Staining techniques are used to detect areas of damage or dryness on the cornea. Our tailored treatment plans, based on specific dry eye conditions and contributing factors, ensure highly personalised care, including advanced in-office therapies like IPL therapy and LipiFlow.
Digital Retinal Photography:
Our technology offers in-depth retinal analysis, capturing detailed images of the retina for a more comprehensive view than traditional methods. With instant results, you can discuss your retinal images with your optometrist. Comparing images from different years helps detect changes over time, guiding treatment decisions. Digital retinal photography can prove beneficial for patients with conditions like high blood pressure and diabetes.
Optical Coherence Tomography (OCT):
OCT enables retinal imaging precision by creating cross-sectional or 3D images of the retina. It is used for early disease detection, identifying eye problems even before symptoms manifest and allowing for timely intervention. OCT can detect macular degeneration, glaucoma and diabetic retinopathy. It also unveils hidden conditions that cannot be seen with standard examinations, all while being non-invasive and safe for visualising underlying layers of the eye.
Corneal Topography:
Our technology enables us to conduct corneal topography, a precise mapping process for the cornea’s surface curvature. Cornea assessment involves mapping the curvature of the clear front membrane (cornea) responsible for significant focusing power. Our technology creates a detailed three-dimensional map of the cornea’s shape, aiding in diagnosing, monitoring and treating various visual conditions. It also identifies visual aberrations like astigmatism, keratoconus and corneal dystrophies that impact vision.
Automated Perimetry:
Utilising the Humphrey Field Analyser (HFA), we can provide automated perimetry assessments. This involves assessing the visual field, detecting blind spots (scotomas) and other visual field defects that may indicate eye and brain issues. The size and shape of scotomas provide insights into the presence and severity of eye, optic nerve and brain conditions. Automated perimetry may identify visual field defects related to conditions such as glaucoma, retinal diseases, optic neuropathy, brain tumours and stroke.
Potential Benefits of Our Technology
Because we at Central Coast Eyecare leverage advanced technology, you may be able to receive the following benefits when you visit us:
- Early Problem Detection: Our technology can pinpoint visual field defects as early indicators of potential eye and brain disorders, allowing for prompt intervention when needed.
- Disease Insights: By analysing the shape and size of blind spots, our technology provides valuable diagnostic insights, aiding in the identification of various eye and brain-related conditions.
- Comprehensive Assessment: Because our technology can produce meticulous data relating to your eye health, we will be in a better position to tailor accurate and effective treatment plans.
- Baseline Comparisons: Establishing a baseline with our technology enables ongoing monitoring of changes in the visual field over time, helping detect and address issues as they evolve.
- Timely Treatments: Our technology helps to quicken the testing process without compromising on accuracy. This can, in turn, eliminate hassle and save you time.
We make sure that all the equipment we use adheres to industry standards.
Get in Touch Today